 Filed Under: Health Economics | Maternal Health
Filed Under: Health Economics | Maternal HealthManaging the Key Cost Lever for Your Maternal Health Program

As many states move to expand Medicaid postpartum care from 60 days to twelve months, the high costs associated with maternal morbidity are in the news.
The term ‘maternal morbidity’ describes any medical or psychological condition aggravated by pregnancy that can negatively impact the quality of a mother’s life – for weeks, months, or even years. Examples include gestational diabetes and preeclampsia. Maternal morbidity can occur during pregnancy or postpartum.
The high cost of maternal morbidity
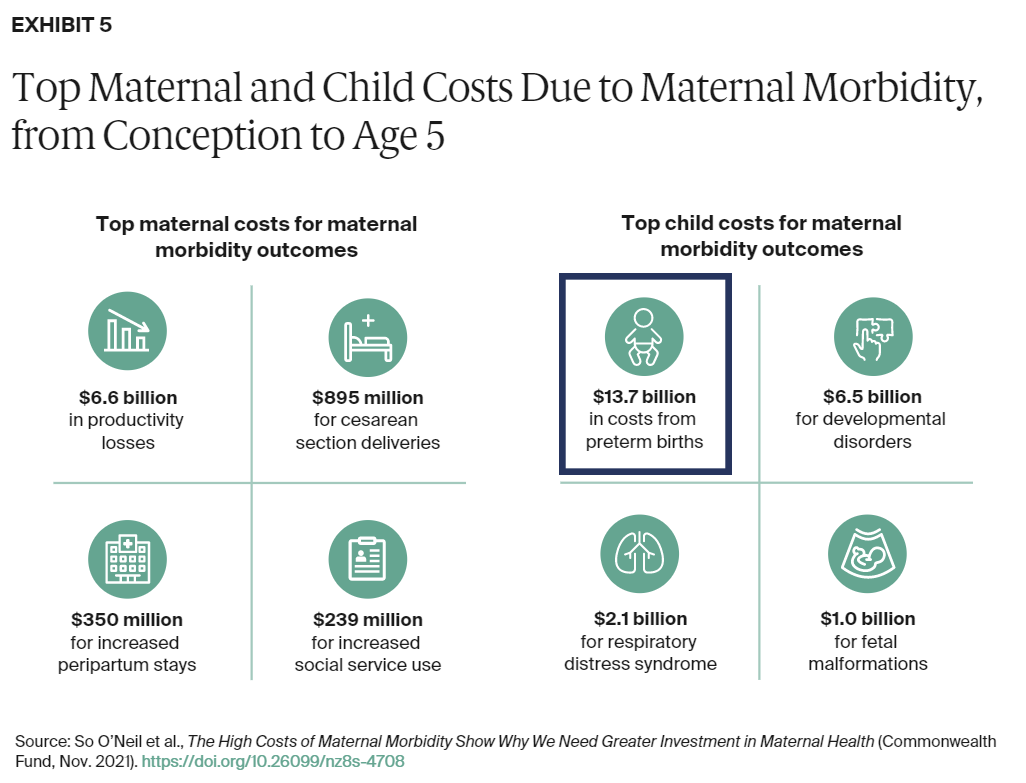
In a recent report, The Commonwealth Fund estimated total maternal morbidity costs for all U.S. births in 2019 from conception through the child’s fifth birthday to be $32.3 billion. When tacked onto normal pregnancies, births, and toddler years, these costs amount to an additional $8,624 for every mom/child pair.1
Two sides drive the costs: the mother’s morbidities (productivity losses, C-sections, longer postpartum stays, etc.) and the child’s morbidities (respiratory distress, developmental disorders, fetal malformations, etc.).
Not surprising to ProgenyHealth, of all these costs, one dwarfs all categories: the $13.7 billion cost of preterm births. Preterm birth costs nearly equal the cost of all others combined.
The NICU savings lever
The Commonwealth Fund report explains why health plans and employers offering maternity programs must also manage NICU cases to manage maternal morbidity costs effectively.
The diagram below sheds light on the trend of implementing maternity programs. The pie chart on the left shows how Well Babies make up the vast majority of births at 86% compared to the small sliver of NICU births at 14%. The pie chart on the right tells the true cost story. For managing costs, NICU represents the overwhelming majority of total newborn spending at 76%. This is the highest cost segment for maternal morbidity highlighted by The Commonwealth Fund report.
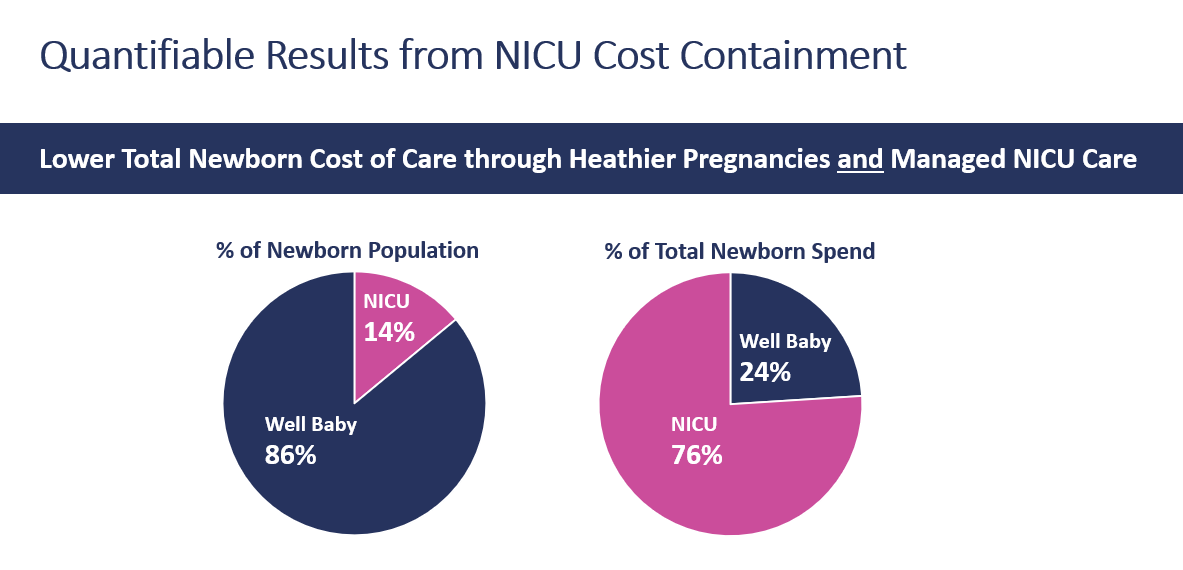
Health plans and employers choose to implement programs that will reduce the percentage of NICU cases. Striving to reduce NICU stays is a critical activity, but only reduces NICU cases incrementally and alone does not achieve the full potential for reducing the cost of maternal morbidity.
Maternity programs educate women during pregnancy, collaborate with physicians, manage chronic conditions that impact a pregnancy, coordinate doctor visits, and solve Social Determinants of Health. These actions can be effective in reducing preterm births. But compared to the measurable savings from a NICU utilization and case management program, savings from maternity programs derived from NICU avoidance alone are harder to quantify. A combined approach – working with the mother during pregnancy plus a holistic approach to NICU care management – offers a better measure of total cost reduction and indicates the maternity program’s effectiveness.
NICU avoidance is part of the rationale for maternity programs. A payer can move a few percentage points of NICU stays into the Well Baby category by providing prenatal monitoring and wellness support.
That small percentage point shift is welcome and substantive but is dwarfed by savings from a NICU Care Management program – savings from expert management of unavoidable NICU cases.
How NICU delivers savings
Should a NICU event occur, ProgenyHealth reduces costs and improves outcomes through multiple NICU savings levers that can be effective in all payment environments:
- Managing length of stay
- Leveling of care
- Appropriate diagnosis codes
- Reducing ER visits
- Avoiding readmissions
“We want to avoid NICU cases as much as possible by getting that baby to a healthier birth,” explains Marcia Wasserman, ProgenyHealth’s Vice President of Strategic Accounts. “But at the end of the day, the big costs are in the NICU. We advise our payer clients to invest in the entire maternity spectrum from pregnancy through the first year of life for mom and child. The greatest return comes from an integrated maternity and NICU care management program.”
Expanded postpartum care also delivers
ProgenyHealth recommends that health plans invest in the entire maternal spectrum – prenatal, NICU, and postpartum – because more than 50% of maternal morbidities occur after leaving the hospital. With ProgenyHealth, our nurses build a trusted relationship with the mother during the pregnancy and continue to monitor the mother’s condition during those critical 12 months postpartum to address issues as they arise. Our nurses ensure the mother has transportation to get to her postpartum visits and identify psychological issues like postpartum depression that can occur throughout the first year.
In April of this year, the CMS announced that funds from the American Rescue Plan were available to extend Medicaid postpartum coverage from 60 days to a full twelve months. ProgenyHealth is helping states’ managed Medicaid partners expand postpartum care for their Medicaid recipients.
ProgenyHealth’s full-spectrum approach reduces the incidence of NICU cases and, importantly, the intensity and cost of the NICU stay. Throughout the pregnancy, ProgenyHealth provides the first line of defense to identify early warning signs for strokes, cardiac conditions, postpartum depression, and various chronic conditions.
Capturing the greatest ROI
Expanding access to postpartum care delivers better outcomes and reduces associated costs. The Commonwealth Fund study found that two-thirds of maternal morbidity costs occurred within the first year postpartum. But for payer organizations looking to reduce their total maternity-related spending, Maternity care programs that include NICU care management consistently deliver the greatest ROI.
- www.commonwealthfund.org/publications/issue-briefs/2021/nov/high-costs-maternal-morbidity-need-investment-maternal-health




 Prev
Prev