2025 Trends Report: Steep Challenges & Uneven Progress
15-minute read
Read how 7 of the most pressing trends in maternal and infant health may shape the months—and years—ahead.
In ProgenyHealth’s 2025 Trends Report, our clinical, financial, and strategic leaders identify the challenges and opportunities that will define the year, for both Medicaid and commercial health plans, including:
- A renewed focus on maternal decision-making
- Advances in neonatology and viability
- A reexamination of employer benefits
We invite you to view the 2025 report
Start Reading
Introduction
The State of Maternal and Infant Health in America

The state of maternal and infant health in America remains precarious. By now, the sobering data has become all too familiar: The United States’ mortality rate is the highest of all high-income nations. Tragically, as many as 80% of maternal deaths, many of which occur in the first 42 days after giving birth, are preventable. The high rate of maternal mortality doesn’t touch every population equally; Black women have the highest rate of maternal deaths in the nation.
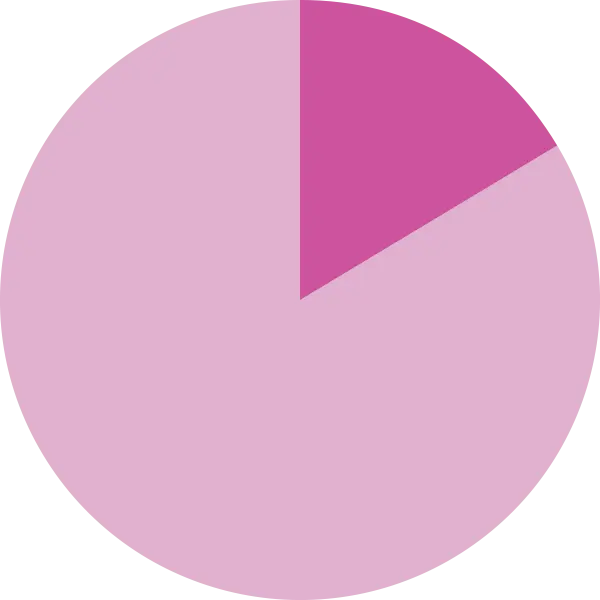
A significant factor in the maternal mortality crisis is a nationwide scarcity of mental health resources: Roughly 20% of new mothers experience Perinatal Mood and Anxiety Disorders (PMADs) within the first year of motherhood, yet only one-third are able to access needed care. Research indicates that approximately 7.4% of pregnancy-related deaths are the result of suicide.
These facts are already deeply troubling, but in the context of the current climate around reproductive issues, they represent a matter of even more grave concern. With multiple states now restricting or banning reproductive care, a spate of new maternal health care challenges has arisen, including reduced access to reproductive care; an exodus of maternal health care providers from those states; and unclear legal mandates hamstringing medical professionals. These factors threaten to exacerbate existing systemic shortcomings at a time when the status quo is already immensely challenging.
But there is hope on the horizon, as an increasing volume of healthcare-focused experts strategize to turn this situation around—and as new trends arrive to disrupt this sector and offer fresh opportunities and solutions. These shifts promise to upend the present state of maternal and infant health, setting the nation on a new path forward.
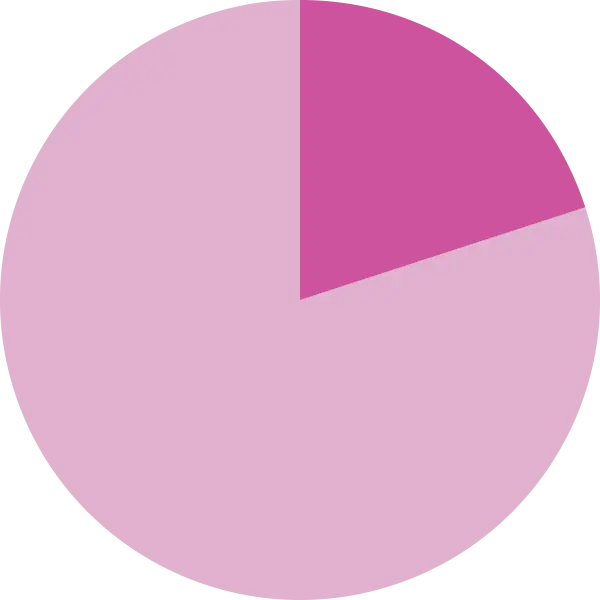
20%
of new mothers experience Perinatal Mood and Anxiety Disorders (PMADs) within the first year
Trend #1
Maternal Decision-Making Will Take Center Stage
The maternal health crisis has at least uncovered one silver lining—the dawning realization that enhancing patient experience and respecting a patient’s self-determination is central to improving maternal outcomes. Increasingly, parents and parents-to-be are getting the message as well, and are seeking to make their voices heard—with primarily positive outcomes. Having a birth plan in place, for one, can be enormously beneficial to both parent and child, resulting in fewer C-sections, shorter labor, and higher APGAR scores for infants.
The concept of self-determination in the birthing process is being taken more seriously by medical institutions, some of which are piloting programs that create a dedicated care team to listen to, work with, and support those going through the birthing process. Some Medicaid states are also looking at similar solutions, as evidenced in requested proposals from Managed Care organizations, focused on patient experience-oriented birth solutions. These programs provide patients with care teams that strategize about the best next steps at each stage of labor and delivery, with the patient involved at every phase of the process—and may well spell the difference between the status quo and a new paradigm of labor and delivery.
They are also giving women a more empowering birth experience. As an example, in 2023, Saint Peter’s University Hospital in New Brunswick, New Jersey, launched its TeamBirth program to improve communication between laboring mothers and the hospital’s clinical team. As a result, the number of patients who said they felt involved in the birthing decision-making process rose from 57% to 88%.
Research shows, providing a more empowered birthing experience for women pays off dividends down the road—including mothers who are more capable of caring for themselves and their babies and of surmounting other life challenges.
Trend #2
Neonatology Will Continue to Advance the Viability of Micro Preemies

Until recently, very few infants born before 26 weeks were likely to survive. Today, many infants born as early as 22 weeks are not only surviving, but thriving, due to inspiring medical advancements.
These micro preemies still only make up 0.3% of all births, but their care can account for a large swath of a health plan’s expenditures, with the mean cost of a micro preemie’s early care falling anywhere from $61,310 to $263,958. Thus, these extraordinary advances in micro preemie care often mean longer, costlier NICU stays at a time when many health plans are already facing immense financial pressures, in part due to Medicare Advantage and Medicaid redeterminations.
In the year ahead, health plans must continue to rise to this challenge and find strategic ways to manage the complex and costly micro preemie cases in their purview. How? By standardizing care, including using small baby programs that efficiently and effectively provide proactive interventions to stave off future complications, and by instituting care management programs that provide families with the support they need to prevent readmission and set early-birth infants on the best possible path.
At ProgenyHealth, our Utilization Management team makes certain that infants receive the best care by ensuring that evidence-based guidelines are followed and they receive the correct diagnosis, the appropriate level of care, and the right number of days in the NICU. Our Case Managers also support families by connecting them to additional resources and providing education on how to care for their medically complex newborns when they are discharged to avoid costly, disheartening, readmissions through their first year of life.
$61,310
to $263,958 is the mean cost range for micro preemie early care
“Innovations, developments and break-throughs in our field have entirely improved the outlook for our young born extremely early.”
Linda Genen, MD, MPH,
ProgenyHealth Chief Medical Officer
Trend #3
Payers Will Increase Focus on Postpartum Support for Women

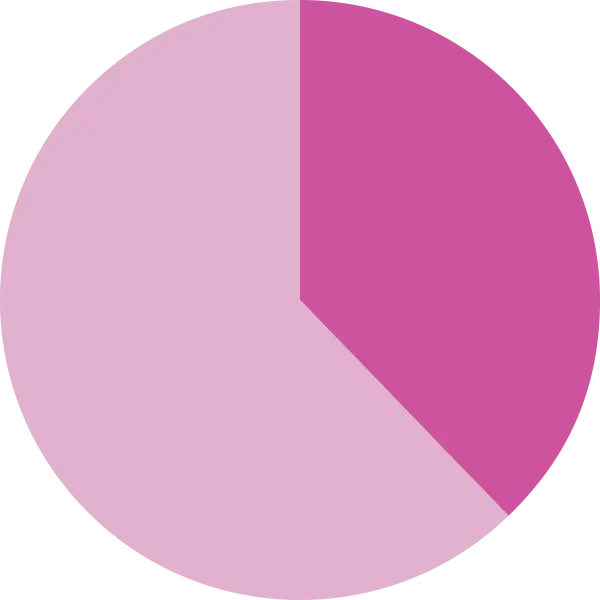
Between 2017 and 2019, nearly 30% of pregnancy-related deaths happened in the six weeks to 12 months after women gave birth, CDC data shows. Notably, many of these deaths were tied directly to mental health issues, which tend to go both undetected and untreated in the postpartum period. In fact, while postpartum depression affects 1 in 7 new mothers in the first year after giving birth, as many as 50% of cases go undiagnosed.
The reality is that physicians and health plans often struggle to extend maternal support during the “fourth trimester,” or first three months after a child’s birth, particularly since many women may have fewer scheduled touchpoints with their provider or may lack basic access to pre- and postnatal care. Indeed, an estimated 2.2 million women of childbearing age live in maternity care deserts, lacking access to OB-GYN services.
Fortunately, most states have now expanded Medicaid coverage for up to 12 months postpartum. And Medicaid Health Plans are helping to improve the postpartum period, particularly for vulnerable communities, in multiple ways, including by leveraging doulas and midwives to address patient mistrust and offer more personalized care.
Research shows that people leveraging doula support are less likely to have preterm births, less likely to experience postpartum depression, and more likely to breastfeed. And among low-risk pregnancies, midwives can help achieve improved health outcomes, including lower rates of preterm births.
Commercial payers are also zeroing in on new thinking around the postpartum period as well. Blue Cross and Blue Shield of Illinois, for example, launched a program, Special Beginnings, with $8 million targeted towards local nonprofits, technology partners, and doula training to improve pregnancy and postpartum outcomes. Meanwhile, Humana’s pregnancy and postpartum care program, HumanaBeginnings, offers services such as transportation to and from doctor’s appointments, newborn support care, and home meal deliveries.
To address the complex needs of the postpartum period, ProgenyHealth works to eliminate barriers to care by providing 12 months of personalized support to all the members we serve. This support includes mental health screenings, as well as clinical recommendations for those in need of further mental health care. By remaining in close contact with members in this particularly precarious moment in their parenthood journey, we can stem the tide of mental health crises and maternal deaths, identifying areas of concern before they become emergent.
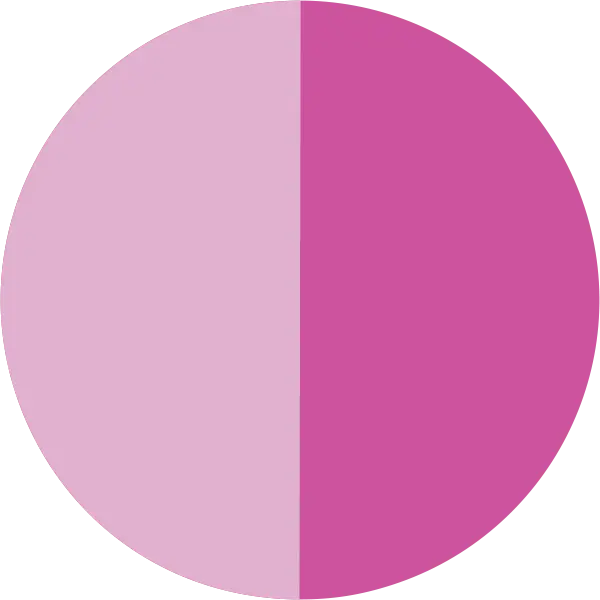
50%
of postpartum depression cases go undiagnosed
The Long Game
Mental health difficulties for parents well beyond the postpartum period also remains a hot topic—and one for which health care experts are still unearthing solutions. Last year, Surgeon General Vivek Murthy released a landmark advisory, Parents Under Pressure, which revealed that 48% of parents report feeling “completely overwhelming” stress most days. As the healthcare industry trains its focus on postpartum mental health, it’s likely that increasing attention will also be paid to the ongoing epidemic of stress and burnout among parents of children of all ages with interventions such as continued mental health screenings.
“As Case Managers, we are conducting outreach to our families to understand how their baby is doing and making sure that they’re hitting the developmental milestones they should.”
Gabrielle Seaman, RN, BSN,
ProgenyHealth Case Management Supervisor
Trend #4
Amid Rising Costs, Employers Will Demand Alternatives to Standard Insurance Products
In late 2024, Kaiser Family Foundation (KFF)’s annual employer health survey revealed an eye-popping statistic: the average annual family insurance premium topped more than $25,000 that year. “Employers are shelling out the equivalent of buying an economy car for every worker every year to pay for family coverage,” KFF president and CEO Drew Altman said in the report. And that number is only expected to increase, with Mercer predicting that per-employee health care costs will climb by 5.8% in 2025.
It’s clear that this financial burden has become untenable for all involved, and that is likely to lead to significant shifts in the collective approach to healthcare coverage in the years ahead.
Since total birth costs are one of the top cost categories for health coverage, employers will likely begin to focus on proactive managed care partnerships to provide additional support during this complex period. An integrated solution not only offers a more comprehensive level of care to members—increasing patient satisfaction and plan loyalty—but it also delivers significant cost savings to employers by identifying and thwarting potential costly conditions before they take root.
This can be particularly useful in the postnatal period, since managed care programs increase patients’ opportunities to report mental health concerns, and because they help to boost the health literacy new mothers need to effectively manage their own care and that of their infants.
Bottom line
More instances of postpartum contact between care provider and new parent equal more chances to intervene and offer guidance when it truly counts.
$25,000
is the average annual family insurance premium
“Employees who take care of premature and complex newborns face financial, emotional, and logistical challenges that impact their ability to bring their best to their jobs.”
Ann Kent, MSW, MBA
ProgenyHealth Chief Growth Officer
Trend #5
Increased Birth Anomalies Will Require More Complex Care

Congenital anomalies are among the chief causes of infant mortality, and as births increase across the nation—particularly in states with reproductive health restrictions in place—these anomalies are expected to climb. In fact, it’s already happening. Data shows that as births have increased after the institution of statewide abortion bans across the U.S., so too have birth anomalies, by as much as 16.6%.
Children born with such anomalies may require surgical intervention, ongoing physical or occupational therapy, long-term educational support, or an array of assistive devices—needs that may evolve and last for life.
Partnering with a healthcare solution with expertise in complex cases like these can be beneficial both to expectant parents and to plans that aim to reduce their financial burden. This is particularly true in states where reproductive health restrictions have made the need for this expertise mission critical.
Early interventions—the necessity of which new parents may only recognize with the aid of an experienced care manager— have been shown to reduce neurological and motor lags common in premature infants. This kind of support represents a clear benefit to the families affected, as well as to the plans covering the cost of their continued care.
16.6%
increase in birth anomalies following statewide abortion bans in the U.S.
Trend #6
Whole Genome Sequencing Will Become a Game-Changer for Newborn Care

Genetic diseases such as Trisomy 21 and spinal muscular atrophy are among the leading causes of neonatal and infant mortality. Many more of these diseases are not fatal but can have a myriad of negative effects on a child’s health. Yet according to one study, only around 38% of women report receiving genetic testing during pregnancy, and even those that do undergo testing are not screened for all possible genetic anomalies.
All of which means that thousands of genetic disorders are likely going undiscovered—either until birth or later in childhood—since many infants may show no signs of genetic anomalies but be carriers of mutations that may impact their health years down the line.
Enter Rapid Whole Genome Sequencing (rWGS), a test for newborns that may soon address this widespread blind spot. The genetic test can be used to identify and diagnose numerous conditions, including developmental delays, seizure disorders, conditions that affect hearing, vision, and immune deficiencies. rWGS is faster and more accurate than other genetic testing and considers a person’s full DNA sequence.
An increasing number of hospitals around the country are now providing rWGS testing on newborns who present with certain signs and symptoms suggestive of a genetic condition, and the results are promising. There are a few state specific programs focused on WGS in the newborn: Baby Bear in California, Baby Manatee in Florida, Baby Badger in Wisconsin and Baby Deer in Michigan.
In 2020, a newborn-focused genetics program launched across several Michigan hospitals, offering rWGS to critically ill neonatal and pediatric inpatients. Administrators found the program spurred early identification of potentially devastating disorders—and accelerated the early interventions needed to improve quality of life. As a result, it helped reduce hospital stay by as many as 214 days, reducing the cost of newborn care by as much as $4,155 per infant.
While rWGS remains unavailable to many families, that situation is likely to change in the years ahead. There are now 15 states that have passed laws ensuring genetic testing coverage for Medicaid members, and both health plans and hospitals are taking note—and instituting new pilot programs to meet this vital need.
38%
of women reported receiving genetic testing during pregnancy
Trend #7
The Rate of Home Births Will Keep Rising—as Will Insurers’ Potential Role in Covering Them

Research shows between 2016 and 2023, the number of home births soared by 60%, now accounting for 2% of all births. The rising trend of home birth is particularly pronounced among Black women. That may be due to a range of reasons, including that Black women are three times as likely to die in childbirth when compared to white women and that 30% of people of color report feeling disrespected after giving birth in a hospital setting.
Given the growing number of home births, some states are now exploring ways in which supporting this birth choice—and making it safer and more routinized, with intervention available in case of emergency—may help to combat certain aspects of the maternal health crisis. For example, New Jersey is currently weighing potential legislation to require health insurers to cover the full cost of home births, such as midwives and doulas who remain present, in case medical assistance is needed.
At ProgenyHealth, our Case Managers have often encountered expectant mothers who wish to give birth at home. We strive to take member preference into account, offering those under our management the agency to pursue the birth plan that’s right for them. However, we also help to ensure that they make safe decisions for both their own health and that of their infant.
As the healthcare professionals all along the continuum of care adapt to the new paradigm of increasingly common home births, they would do well to take a similar tack. Such an approach would involve accommodating the wishes of the patient as much as possible while also ensuring safe conditions, offering labor and delivery guidance whether in person or in advance, and encouraging those in labor to escalate the situation if a hospital transfer is warranted.
+20,000
Increase in home births between 2016 and 2023
Conclusion
Bracing for Change, Together

The data tells a sobering story, underscoring the critical need for continued efforts in the healthcare realm to secure brighter futures for mothers and infants. With a new administration taking office in 2025, health plan executives are bracing for shifts in the healthcare landscape—further emphasizing the importance of steadfast commitment and collaboration in the path forward.
At ProgenyHealth, we take pride in being on the front lines of this mission, providing essential support and guidance to new parents, while contributing to an industry focused on groundbreaking advancements and innovation. While the road ahead is filled with an imposing set of challenges, it is clear the policies and people necessary to change course are ready and willing to make a difference.
“2025 is poised to be a year in which health plan leaders and policy makers embrace innovative solutions to write a new chapter in our country’s ever-evolving story of maternal and infant health.”
Susan Torroella, MBA
ProgenyHealth Chief Executive Officer
About ProgenyHealth
ProgenyHealth empowers our health plan and employer partners to change the trajectory of maternal and infant health outcomes across America. Informed by more than 20 years of experience and patient data, our end-to-end maternal and infant care management solution helps ensure the best possible outcomes for every expecting mother we touch.
Our wholly integrated, tech-enabled solution builds a network of support for an uninterrupted continuum of care from prenatal health, through any resultant NICU stay, and all the way to one full year of life. From the very beginning, we unite early health risk assessment data with self-directed digital tools and dedicated case managers who work tirelessly to connect at-risk moms-to-be with the resources, care, and support they need for a healthier, full-term delivery.
By promoting predictable, equitable, and standardized high quality care journeys, we ensure healthier outcomes—and lower costs—across an entire at-risk population. In so doing, we help overcome systemic barriers to support healthier pregnancies and healthier starts to life for all moms and babies, one family at a time.

