5 Keys to Successful Member Engagement
10-minute read
Extending the Reach of Health Plans through Trusted Best Practices
Start Reading

Extending the Reach of Health Plans through Trusted Best Practices
Member satisfaction has long been a holy grail for commercial health plans and Medicaid Managed Care Organizations (MCOs). Yet, after years of investment to improve the member experience, fewer than half (45%) of insured people surveyed last year said they were ‘fully satisfied’ with their health coverage.
That same survey found that members sought better engagement – a metric underscored by the 85% who felt more satisfied when health plans communicated in their preferred way.
When asked how health plans can improve, the answers included:
- “High-quality customer service”
- “Easy access to medical records”
- “Tools and information to avoid high-cost care”
- “Connecting me to providers based on my preferences.”
Taken together, high engagement drives member and provider satisfaction, improves overall health outcomes, and retains members.
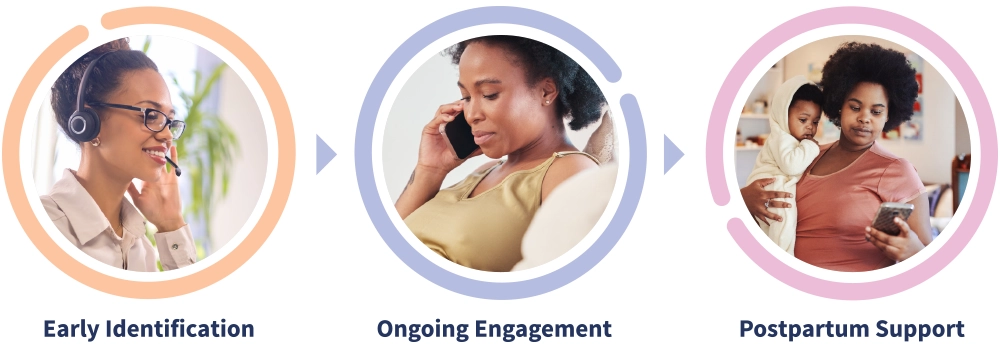
Successful member engagement is especially important for health plans supporting pregnancies and potential NICU admissions. Timely notification of a pregnancy and sustaining engagement create unique hurdles. Once health plans identify pregnant members, maintaining consistent engagement across critical touchpoints becomes a challenge. Most importantly, members who aren’t engaged can miss out on recommended prenatal and postpartum care. Should a NICU admission occur, engagement is critical to providing support and education, building self-advocacy in caregivers, and reducing avoidable readmissions via the establishment of discharge plans that support transition from the NICU to home.
Staying Engaged: A challenge for commercial health plans and Medicaid MCOs
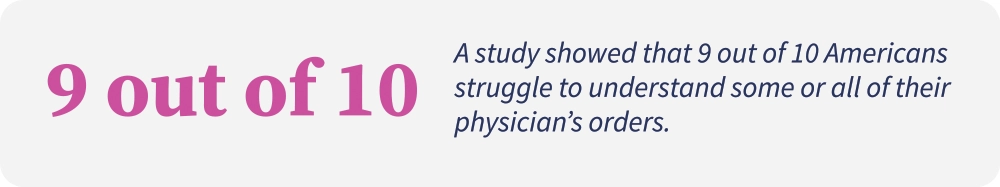
As multiple studies have found, offering excellent benefits doesn’t necessarily translate to engagement. Like any relationship, communication is key. Case in point, a Forrester survey explored reasons engagement suffered: 41% of consumers wanted their plan to communicate their benefits more clearly, and 31% found their plan’s website hard to navigate.
While websites and digital apps can help with engagement, members at the highest risk often need one-on-one support. In a 2023 study by J.D. Power, only 17% of commercial members with a self-reported health status of “poor and fair” were assigned a case manager. With many of these members working with multiple providers and a similarly high number of medications, there is an increased risk for a lack of coordination, leading to poorer health outcomes and higher spending.
A government report on Medicaid member engagement found that 7 million eligible people could lose coverage because of “administrative churn” – a catch-all term for someone who moved, changed their phone number, or couldn’t make an appointment because of work, transportation, or childcare needs. Administrative churn is also commonplace among pregnant women.
Engaging pregnant women through the entire care journey is critical to identifying high-risk pregnancies sooner, intervening earlier, and avoiding pre-term births and pregnancy complications. Engagement challenges grow exponentially when mothers face financial, language, transportation, and other care barriers or distrust the healthcare system.
Commercial and Medicaid: Same goal, different challenges
Pregnant members in both commercial health plans and Medicaid MCOs face challenges, but their needs may vary.
- Both populations face challenges around anxiety and depression, health literacy, and accessing care.
- Healthy members present a different kind of challenge. “Feeling fine” becomes a reason to avoid taking advantage of covered services.
- While Social Determinants of Health (SDoH) issues may be more visible when working with Medicaid members, many commercial plan members also face financial, housing, food, and other types of insecurity.
- Furthermore, both populations are likely to experience many of the same clinical issues, including high blood pressure, BMI issues, infertility, substance use disorders, domestic abuse, and LGTBQ+ concerns.

Engagement: New challenges for health plans
A Forrester report found that most health plans struggle to offer seamless digital experiences. The report mentioned:1
- The lack of visibility and clear member communication in the digital space.
- The inability to find information online if a phone call is insufficient.
- Failure to adequately measure member sentiment or track their start-to-finish journey.
Fierce Healthcare also found engagement pitfalls that plans should avoid:2
- Targeting the wrong members. Instead, focus on those who have chronic conditions, open care gaps, or are unengaged in their health.
- Using the wrong communication channels, for example, sending mail to members who prefer digital or mobile.
- Focusing on the wrong activities instead of activities most likely to improve members’ health.

Five Keys to Successful Engagement
Lessons learned from over 20 years of experience
1. Communications and outreach must be relevant and show empathy
- Start early to build rapport before complications arise.
- A one-size-fits-all approach to outreach will feel cookie-cutter to your members, especially if the Case Manager does not demonstrate empathy and understanding for their situation.
- Many health plans have an outreach team that is script-driven and condition-agnostic. The need to assign an assessment must be balanced with the value of engaging with the member. This is where active listening on behalf of the Case Manager becomes critically important.
- Provide members with options that allow them to personalize their experience. Because health is personal and intimate, many members may wish to talk to a nurse every time. For members seeking information independently, a mobile app might be a better choice.
2. Outreach must be multi-channel and persistent throughout pregnancy and postpartum
- Members won’t take advantage of included benefits if they are not aware they exist. Ongoing communication ensures that members understand a valuable program and know how to access it when they are ready to engage.
- Members take great comfort in knowing their health plan has their back for the entire journey.
- Even if communication is missed or a member feels the program isn’t necessary, a need may arise later when the member needs to know where to turn.
- A multi-channel approach keeps benefits top of mind.
3. Support should also be multi-channel
- Some people are more comfortable communicating by phone, while others prefer text, email, or apps. Letting the members decide which form of support they prefer extends engagement to more members.
- Cultural competency is equally essential for engagement. Understanding the member’s needs and meeting them there improves engagement and outcomes. Member materials must be written in the languages representing the communities members live in.
- By building relationships with community-based organizations such as food and diaper banks, health plans can deepen their investments in communities, while strengthening their ability to respond to the non-clinical needs of members.
4. Program offerings are a form of engagement
- Members feel more engaged when they feel the plan supports them. When the plan covers the services, resources, and conditions associated with maternity care – including preeclampsia, gestational diabetes, and obesity – loyalty increases dramatically.
- Members with high-deductible plans must balance medical needs versus out-of-pocket costs. Including more benefits becomes a competitive differentiator.
5. Establish trust
- ProgenyHealth’s dedicated Case Managers connect with mom and infant to act as trusted advocates, identify and solve needs, and offer educational and emotional support during a trying time.
- The overriding goal is establishing trust – especially at the beginning of the engagement. If the member is confident that the Case Manager will be there throughout the journey, they will keep returning if they have issues.
- This bond of trust keeps the member connected throughout the pregnancy and helps proactively identify rising risk.
- Similarly, A NICU admission can be an intensely stressful situation. Given the complexity of the medical conditions that may exist, having a go-to expert to provide guidance can make a substantial difference.
Connections: The Essence of Engagement
When it comes to shaping the journey of a member, health plans have a big say in what it all looks like. But success or failure hinges on the right timing, messaging, and having a strategy that wraps it all together.
Below are just a few of the key ways ProgenyHealth builds trust and communication in service of healthier outcomes:
Leveraging technology
Research shows that nearly two-thirds of pregnant individuals would prefer fewer visits to the OB, and for low-risk members, fewer prenatal visits doesn’t equate to worse outcomes. With virtual monitoring, members don’t have to miss work or juggle childcare. This virtual model of care often involves at-home weight, blood pressure, fetal heart monitoring, and frequent phone-based check-ins with nurses or doctors throughout the pregnancy.
A high-touch, high-tech model of care
ProgenyHealth’s high-touch model of engagement throughout pregnancy, postpartum, and NICU admissions helps ensure a continued source of help and support. Our Maternity Mobile App offers an additional resource for information and support.
Engagement on day one
Regardless of how contact is initiated, establishing trust at the very beginning gives the member confidence that someone in whom they can confide is on their side. During that first one-on-one call, the Case Manager can tap into insights provided by things like mobile app usage data. Perhaps the member was reading articles in the app on nausea or headaches (a warning sign for preeclampsia). The Case Manager also establishes an appointment schedule, explores potential SDoH and behavioral health issues, and discovers whether the member is a candidate for complex Case Management. When assisting families with infants in the NICU, the Case Manager will help with understanding medical instructions or secure special medical devices that may be required after discharge.
Our Case Managers undergo cultural competency and bias training to be trusted confidants. Most importantly, they establish a relationship with the pregnant member as an advocate. The Case Manager underscores that ProgenyHealth will be there through NICU (if needed) and postpartum.
Solving problems in the moment
When a pregnant member is on the phone with ProgenyHealth, the Case Manager tries to solve as many issues as possible, including clinical needs, appointments, and SDoH issues in the moment. Sending members into an IVR phone system can quickly try a member’s patience. If they hang up, the opportunity for engagement is lost.
A True Story of Member Engagement
ProgenyHealth engages mothers-to-be on a comprehensive maternal journey from pregnancy through the first year of life. Our Case Managers forge strong connections with at-risk mothers-to-be to proactively identify clinical and non-clinical health risks and create personalized care plans. As tireless advocates, we provide actionable, real-world support that builds unparalleled trust and earns lasting member engagement.
As a result, our partners’ populations experience proactive SDoH interventions, higher rates of full-term births, and lower incidence of NICU utilization.
Key to all of this is a commitment to always putting the member first. We invite you to read “A Maternity Member’s Journey”. Learn how Maria engaged with ProgenyHealth to manage her high-risk pregnancy – starting with ProgenyHealth’s Maternity Mobile App, moving into close monitoring by our Case Managers, and finally receiving 12 months of postpartum support for her complex SDoH issues.
Read the eBook:
A Member’s Maternity Journey with ProgenyHealth
Learn how Maria engaged ProgenyHealth to manage her high-risk pregnancy – from maternity app and nurse case managers to twelve months of postpartum support for her complex SDoH and behavioral issues.
About ProgenyHealth
ProgenyHealth empowers our health plan and employer partners to change the trajectory of maternal and infant health outcomes across America. Informed by more than 20 years of experience and patient data, our end-to-end Maternal and Infant Care Management solution helps ensure the best possible outcomes for every expecting mother we touch. Our wholly integrated, tech-enabled solution builds a network of support for an uninterrupted continuum of care from prenatal health, through any resultant NICU stay, and all the way to one full year of life. From the very beginning, we unite early health risk assessment data with self-directed digital tools and dedicated case managers who work tirelessly to connect at-risk moms-to-be with the resources, care, and support they need for a healthier, full-term delivery. Our industry-leading intelligent platform, Baby Trax®, integrates NICU Utilization Management and Case Management, while also driving NICU Payment Validation & Assurance activities based on clinical data. By promoting predictable, equitable, and standardized high quality care journeys, we ensure healthier outcomes—and lower costs—across an entire at-risk population. In so doing, we help overcome systemic barriers to support healthier pregnancies and healthier starts to life for all moms and babies, one family at a time.
- Report: Most health plans are struggling to provide a coherent online experience for members – MedCity News
- Industry Voices – 3 member engagement pitfalls health plans should avoid | Fierce Healthcare

