Navigating The Complexity of NICU Care for Micro Preemies
Personalized, end-to-end care management ensures micro preemies and families are supported early, and babies continue to progress and thrive
Learn how ProgenyHealth works with health plans to:
- Provide personalized care management, parental engagement, and physician collaboration quickly and seamlessly to ensure that babies and caregivers receive the support they need.
- Bring a hands-on NICU care management approach to deliver positive outcomes for families throughout their NICU stay.
- Ensure clinical care aligns to the care level assigned by the medical provider, from length of stay to level of care.
- Ensure families are supported, up to one year of life, preventing unnecessary NICU readmissions and helping to reach developmental milestones.
Start Reading
Partnerships are key as health plans manage escalating costs, even as advances improve outcomes for the most vulnerable newborns
The last four decades have seen a tremendous leap in Neonatal Intensive Care Unit (NICU)-related advances. For the most fragile of these infants, dubbed “micro preemies,” their survivability until recently was only possible from 26 weeks, or about six months of gestation. Fortunately, advances in care have given infants as young as 22 weeks, once unlikely to survive, a real opportunity to develop and thrive.
“Innovations, developments and breakthroughs in our field have entirely improved the outlook for our young born too early,” says Linda Genen, MD, MPH, Chief Medical Officer of ProgenyHealth, a leading, tech-enabled women’s healthcare company dedicated to maternity and NICU care management.
Genen credits today’s better NICU outcomes to standardized processes and new technologies, citing enhanced respiratory support, new monitors for oxygen saturation, phototherapy, brain imaging techniques, kangaroo bonding and advanced nutritional support, as some of the breakthroughs. Additionally, the development of “Small Baby Programs”, built to treat infants born weighing less than 1,000 grams, have helped to standardize care.
But even with these advancements, these preterm infants still face daunting health challenges. According to neonatal care specialists, micro preemies are born with very underdeveloped brains and other organs not ready to function outside the womb. They cannot breathe effectively or swallow. Some weigh as little as one pound and sometimes even less.
Preventing injury to the developing brain is a major priority at Stanford Medicine Children’s Health, which houses high-risk infants born before 29 weeks of gestational age in a special small baby unit that uses “specially designed protocols to protect their fragile brains, advanced equipment to help support their lungs and special feeding and nutrition approaches to help babies grow.” A similar program at Brigham and Women’s Hospital in Boston pairs a dedicated neonatologist with each infant throughout their NICU stay.
At University of Iowa Health Care Stead Family Children’s Hospital, speed and precision of care have led to higher survival rates for extremely premature babies compared to those born at other U.S. hospitals. A better understanding of the postpartum challenges of these infants has led providers to work proactively before delivery, implementing prenatal interventions. Noninvasive diagnostics such as echocardiograms via ultrasound machines can examine the micro preemie’s heart and circulatory system and perform precise medical calculations to “mimic the intrauterine environment.”

According to neonatal care specialists, micro preemies are born with very underdeveloped brains and other organs not ready to function outside the womb.
The challenging U.S. maternal and infant health landscape
While these healthcare advances are exciting, the U.S. lags other developed countries in infant and maternal mortality, driven in large part by issues of access to care and health equity. A 2023 study found the U.S. infant mortality rate increased between 2021 to 2022 to 5.6 deaths per 1,000 live births, much higher than peer nations like Sweden (2.2), the United Kingdom (3.7), and Iceland (1.4). What’s more, over 2.2 million women in the U.S. live in “maternity care deserts”, lacking access to necessary prenatal care, and some 51% of counties in the U.S. lack practicing obstetricians. That’s alarming given the correlation between health challenges for newborns when women don’t receive prenatal care.
Having a micro preemie also places a heavy burden on working families in terms of absenteeism from work if they’re even able to remain employed, since one parent may need to stop working outside the home to devote all their time to their extremely premature baby’s care.
For micro preemies, survival can take on many different forms. From long NICU stays to a multitude of comorbidities, the road to discharge is complex and expensive. Beyond the NICU, little information is available on the lifelong cost impacts associated with conditions present in micro preemies. The nearer-term developmental impacts are better known.
“When you’re born early, you are at risk for having developmental delays,” observes Gabrielle Seaman, RN, BSN, a case management supervisor for ProgenyHealth. As a former NICU nurse, she’s seen the challenges families face firsthand. “As a case manager, we are conducting outreach to our families to understand how their baby is doing and making sure that they’re hitting the developmental milestones they should.”
It has taken decades of tireless research, technological breakthroughs, and a commitment to providing previously unimagined levels of care, but families are now seeing the lifesaving benefits for the tiniest members of our society. And while this is cause for much celebration, the reality of corresponding complex care, developmental delays, and yes, staggering costs, must be addressed. Unsurprisingly, many health plans have been challenged by the complexity of these cases. Who should health plans turn to if they are determined to provide the best possible outcomes while also controlling costs?

From long NICU stays to a multitude of comorbidities, the road to discharge is complex and expensive.
The Solution: Proactive, specialized care management
NICU case management can serve as a lifeline for families in managing the complexity of care for their preemie, from getting key support resources to knowing how to care for their baby post-admission.
“It’s a very vulnerable time for families, so giving them the support they need whether that’s a community resource or solving a problem, is key,” says Seaman, noting that one of the biggest problems her case managers see is transportation as a barrier for the family. “We connect those families with transportation services and other benefits early on, which sets up the family for success later,” she explains. Other issues that arise include ensuring follow-up appointments to address all the medical needs of the premature infant are met, medication education, and securing medical equipment for the home environment just to name a few.
ProgenyHealth’s team of utilization management experts provide physician/nurse collaboration during the inpatient stay, as well as personalized case management with parental engagement to ensure healthier outcomes and better experiences for all involved.
Seaman says it’s critical to engage with families early and continue to monitor the baby’s progress up to the infant’s first birthday because “sometimes you don’t see those delays until later on down the line when the baby is six or eight-months old.”
For this reason, she and other staff prioritize outreach to families to make sure they make all scheduled well child visits within that year, and vaccinations are done to prevent re-admissions to the NICU. “Our Case Managers educate parents on how to care for their NICU baby upon arrival home and take the time to explain the use of durable medical equipment to prevent re-admissions,” explains Seaman.
Current research shows that preterm birth rates and NICU utilization among infants born in the U.S. are on the rise. According to a cohort study using linked data published in July 2024 in The Journal of Pediatrics, 8.5% of all infants with very low birthweight born in California from 2009 to 2018 and discharged from NICUs in California were readmitted within one month of discharge.
A 2023 study found the U.S. infant mortality rate increased between 2021 to 2022 to 5.6 deaths per 1,000 live births, much higher than peer nations like Sweden (2.2), the United Kingdom (3.7), and Iceland (1.4).
Personalized engagement: NICU integrated care in action
One mother of a 22-week-old micro preemie expressed how much she appreciated the support provided by ProgenyHealth’s case management team. “I love the fact that I’m not alone in this process. It means a lot. Support-wise, this is amazing, and we need that,” she said, noting that her case manager helped clarify her baby’s conditions, ranging from retinopathy, which causes the retina of the eye to detach, to a hernia. The ProgenyHealth case manager also offered guidance for securing needed items like a car seat and crib when her baby was ready to come home.
ProgenyHealth’s case management team helped her get these items through her health plan, as well as gas reimbursement. The team also identified a mentor through a non-profit, coordinated by volunteers who empower and support families of fragile infants.
Re-admissions are common and cumulatively cost the U.S. healthcare system millions of dollars per year, creating a significant burden on the healthcare system. The study further found that compared with those with no readmission, infants readmitted within 30 days of discharge were more likely to have lower birth weight and higher rates of chronic lung disease and any surgery during admission. Their mothers were more likely to have less formal education, to have public insurance and more likely to reside in less advantaged neighborhoods as defined by the Child Opportunity Index.
“Families with infants in the NICU go through a lot during that initial stay and being readmitted shortly after discharge is a major setback both emotionally and financially for them,” said the study’s lead author John Feister, MD, MS, assistant professor of Pediatrics at the University of Cincinnati College of Medicine and neonatologist at Cincinnati Children’s Hospital Medical Center.
He emphasizes that addressing medical risk factors alone is not sufficient. “We need to consider sociodemographic factors such as health literacy and poverty in addition to traditional medical factors when we think about how to reduce the risk of readmission for the infants, we care for in the NICU. We must do a better job of supporting our families via individualized discharge preparation, connection with community resources, and providing post-discharge follow-up care.”
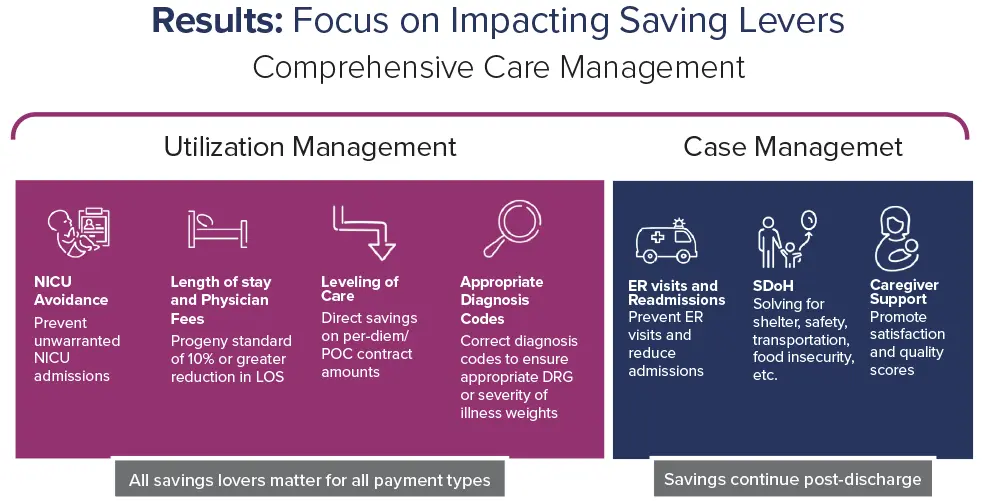
End-to-end, specialized care management is critical for families facing the need for NICU care. At ProgenyHealth, NICU Care Management includes two components: NICU Utilization Management and NICU Case Management. While NICU Case Management teams work directly with supporting the family through the NICU stay, specialized Utilization Management team members work with clinical teams to manage appropriate levels of care and length of stay for their most fragile patients.
“Our Case Managers educate parents on how to care for their NICU baby upon arrival home and take the time to explain the use of durable medical equipment to prevent re-admissions.”
Gabrielle Seaman, RN, BSN,
Case Management Supervisor
ProgenyHealth
Maggie Knaresborough, RN, BSN, a utilization management supervisor, says a big part of her job is ensuring the level of care the provider is requesting for a NICU preemie “actually meets the intensity of service that the baby is receiving in the NICU.”
With its NICU expertise, ProgenyHealth clinical staff and Utilization Managers understand what is happening with the baby by looking at the clinical information and ensuring it aligns with the care level the provider has assigned.
According to Knaresborough, another area that her team monitors is the length of stay for babies. “It’s important that we’re managing the infants throughout the continuum of their stay and ensuring that they have a safe and timely discharge. It’s equally important to understand when those critical milestones should be occurring and making sure that those things that we’re expecting for a NICU infant to be experiencing, based on their gestational age, happen and, if not, work to understand why they’re not moving along that continuum.”
While ensuring appropriate levels of care and timely discharge can have a cumulative cost-savings effect on health plans, the Utilization Management team at ProgenyHealth has also seen a downstream effect on families. Knaresborough has witnessed how family care decisions for their preemie can be adversely affected when medical costs aren’t contained.
“We have seen scenarios where a baby’s readmitted because a formula is being diluted because of the cost, and similar actions that can really impact a newborn’s health,” says Knaresborough. “If families are put in that position, they’re making those choices and those decisions because of the financial impact of that NICU stay and all those other factors that can impact the financial well-being of a family.”
Keeping Costs Down: Payment validation and assurance
Fortunately, cost savings can be “really significant” depending on how savings levers are managed. Another important component of ProgenyHealth’s approach is NICU payment integrity or NICU Payment Validation and Assurance. Health plans depend on the PVA team, which includes NICU-experienced certified medical coders, who apply their expertise to validate whether the diagnoses assigned are supported (ensuring that health plans don’t overpay for an already costly case). They document any variances and include a detailed explanation and rationale for any recommended adjustments. The team also verifies that the room and board revenue codes and units reflect clinical authorizations.
Claims and clinical data are matched directly with Baby Trax®, ProgenyHealth’s industry-leading intelligent medical management platform that integrates utilization management and case management activities. By avoiding the need to request an entire medical record from providers, the platform reduces members’ administrative burden.
The power of ProgenyHealth’s NICU Care Management program is the end-to-end journey through utilization management, case management, and PVA. All these capabilities go hand-in-hand with improved quality, better experience and total cost of care savings, to best serve health plans’ members and families, and ultimately assure that newborns who leave the hospital continue to progress and thrive.

The power of ProgenyHealth’s NICU Care Management program is the end-to-end journey through utilization management, case management, and PVA.
Timely risk detection can lower risk and improve outcomes for preterm births
ProgenyHealth’s proactive relationship-driven approach for families extends to expectant mothers through its Maternity Case Management program.
ProgenyHealth offers comprehensive case management and holistic support that women and infants need, from pregnancy up to 12 months postpartum, led by an interdisciplinary team of obstetricians, neonatologists, pediatricians; maternity, pediatric and NICU nurses; social workers and lactation specialists. These specialists collaborate to help solve for complications before a woman faces the crisis of a very preterm birth. Case managers reach out to eligible pregnant members to enroll in ProgenyHealth’s maternity mobile app. The mobile app helps to assess pregnancy risk levels, which informs our Case Management team members on outreach cadence. Members can make to-do lists, learn about their pregnancy and track progress via personalized care plans. In addition, CMs perform risk assessments to determine if an expectant mother is at a higher risk for having a preterm baby.
Engage with the right partner, early
The U.S. has come far with neonatal advances, even as the complexity of care and long-term costs associated with very preterm births continue to rise. To manage this complexity and ensure positive infant outcomes, health plans need trusted partners who can offer specialized, end-to-end care management—a true expert to understand how to mitigate risk with a whole-person approach through the maternal and NICU journey.
It’s important to bring the right partner in early to ensure the best possible outcomes—an expert who can build trusted relationships with both clinicians and families to champion wellness and proactive care, so babies hit developmental milestones and don’t face ER visits or NICU readmissions. At the same time, with exploding healthcare costs, health plans need a partner that understands the NICU environment well, has the clinical expertise to help ensure payment integrity, and employs smart savings drivers to contain healthcare costs without sacrificing quality of care.

