Today’s Business Imperative: Prioritizing Family-Focused Benefits
10-minute read
How health plans can improve health outcomes, employer and employee satisfaction, and the bottom line via maternity and infant care management.
Employers are enhancing family-focused benefits to attract and retain talent, recognizing the value of supporting employees through pregnancy and early parenthood. ProgenyHealth’s integrated Maternity and NICU Care Management program improves health outcomes while reducing healthcare costs. Case managers guide employees through pregnancy and postpartum, addressing risks such as preterm birth and maternal complications. These benefits also contribute to greater employee satisfaction, stronger retention, and more efficient healthcare utilization.
What you will learn:
-
The Importance of Family-Focused Benefits – How Maternity and NICU Care Management improves employee satisfaction, health outcomes, and talent retention.
-
How Comprehensive Care Management Programs Work – The role of Case Managers in guiding employees through pregnancy, postpartum, and potential NICU stays to reduce health risks and costs.
-
Employer & Health Plan Advantages – How investing in maternal and infant care benefits leads to improved employee retention and loyalty.
Start Reading

How health plans can improve health outcomes, employer and employee satisfaction, and the bottom line via maternity and infant care management.
A New Benefits Landscape
It’s no secret that attracting top talent has become an increasing challenge for employers nationwide. A full 71% say they routinely struggle to locate the skilled talent they need, and a significant number are working to make their open positions more enticing, with 28% raising salaries and 20% offering greater flexibility.
Other employers, however, are turning toward their benefits portfolios, revamping these offerings to draw in the best and brightest in their fields. Perhaps that’s why, since 2022, the benefits landscape has seen major growth, with the variety of offerings increasing by 23%. Indeed, last year 81% of employers said they planned to add to or enhance their benefits portfolios to make their organizations more attractive to new hires.
Shrewdly, many benefits leaders are ensuring that these expanded offerings are healthcare-related, pertaining particularly to the health of an employee’s family. Family health benefits are a distinct priority for many workers, with 94% saying they consider these benefits either important or extremely important. Promisingly, a recent survey indicates that 37% of employers to focus on maternity and newborn care support in their benefits offerings, and 43% aim to better educate their employees on the availability of women’s and family health benefits.

Yet despite this impetus among employers, six out of ten employees say they find fault with their current company’s approach to family-oriented benefits. It’s clear, then, that a gap is forming—between what current and prospective employees want and what is being offered to them, between what companies hope to achieve by revamping their benefits packages and what they’re truly accomplishing, and between the health-related business benefits that organizations could be reaping and what they’re unfortunately leaving on the table. This is where the expertise of health plans can make a meaningful difference.
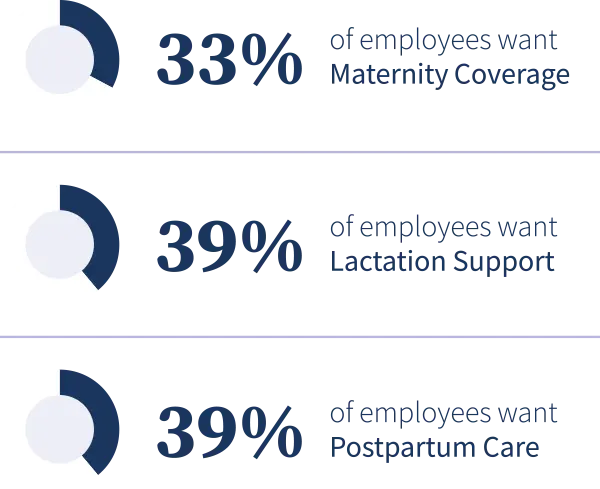
Desired Family Health Benefits
A 2023 study conducted by Mercer identified the following health benefits as “helpful to me or my family”.

What a Comprehensive Maternal & Infant Care Program Can Offer
Research has shown that those with access to care management programs focused on maternal and infant health see more positive outcomes than those without, particularly when it comes to rates of preterm birth.
Leading factors in preterm birth include maternal behaviors like smoking or alcohol use, and chronic conditions such as diabetes, high blood pressure, and stress, all of which are managed within a comprehensive care management program. Put simply, pregnant members—and by extension, their infants—fare better when they have continuous support throughout their pregnancy and postpartum journey, guiding them toward healthy behaviors, as well as proactively identifying, addressing, and solving gaps to reduce their impact on maternal and infant health outcomes.
What does that look like in practice? Let’s say an employee with access to maternity and NICU care management through her company discovers she’s pregnant. She downloads the mobile app and answers questions about her pregnancy. The Case Manager receives this information and reaches out to the employee. This initial outreach takes place telephonically, reassuring the employee that they are speaking with a real person. Through a thorough risk assessment, the Case Manager identifies any potential risk factors—in this example, the employee mentions that she has a history of high blood pressure and has not yet chosen an OBGYN.
From here, the Case Manager suggests a few provider options in the employee’s vicinity, making sure to highlight those who accept her insurance and are in-network. The Case Manager also explains that high blood pressure can lead to a condition known as preeclampsia, educating the employee on the need for regular prenatal visits to keep this condition monitored and under control. Additionally, the Case Manager will provide positive reinforcement on the importance of monitoring the employee’s blood pressure outside of a healthcare setting. As new needs arise throughout the employee’s pregnancy—locating a specialist for a test ordered by her OBGYN, say, or finding local birthing classes—the Case Manager steps in to assist, continuing to identify any risk factors that may arise and coordinating care across providers to reduce gaps in access, all the while ensuring the employee is empowered to make healthy decisions and advocate for their own care. This care management continues during the postpartum period, during which a high preponderance of maternal complications can occur.
Should a NICU admission occur, a NICU Case Manager is assigned to the employee and infant. In coordination with the Maternity Case Manager, the NICU Case Manager connects during the inpatient stay to assess needs and collaborate with hospital staff to support the transition from the hospital to home. They provide education and support, screen for postpartum depression, and help solve SDoH challenges. Case Managers are available to help families ensure continued care with their pediatrician by reducing unnecessary emergency department visits and unplanned readmissions.
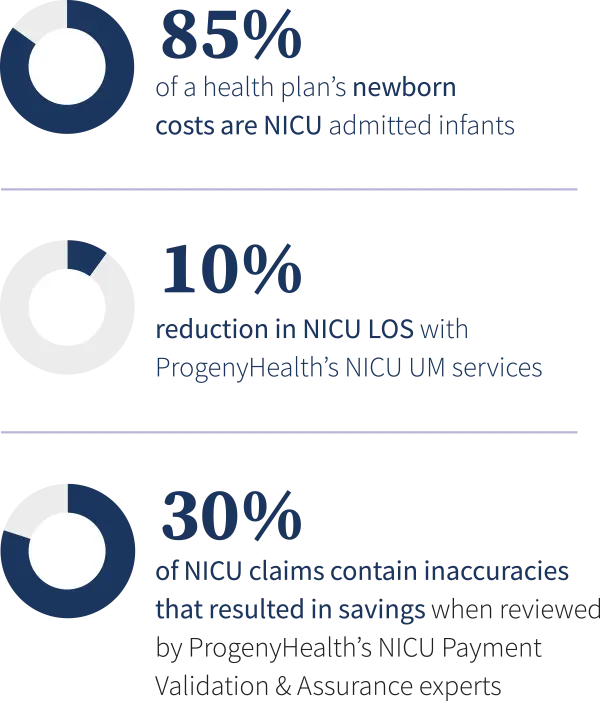
Because a staggering 85% of a health plan’s newborn hospitalization costs comes from infants admitted to the NICU, behind the scenes, the ProgenyHealth NICU Utilization Management team plays a critical role in managing the particulars of the infant’s case. This aspect of the process ensures that the NICU stay is warranted, and the level of care provided is appropriate. They ensure that the infant is progressing using evidence-based guidelines. ProgenyHealth’s NICU Utilization Management has been shown to reduce NICU Length of Stay (LOS) by an average of 10%, meaning infants are discharged and transitioned safely to home and their families more quickly. Additionally, 30% of NICU claims contain inaccuracies that resulted in savings when reviewed by ProgenyHealth’s NICU Payment Validation & Assurance experts, the correction of which can result in significant savings for the employer or health plan. This is particularly important for employers with self-funded health plans.
In all, this comprehensive approach to care management offers a multi-pronged benefit, ensuring quality care, avoiding negative health outcomes, and reducing overall cost of care to ensure maximum savings.
Employees Access ProgenyHealth’s Maternity & NICU Care Management Program in One of Three Ways

Employee
Maternity:
Employee self-enrolls via mobile app/telephone (or) receives outreach call from Maternity Case Manager
NICU:
Employee receives outreach call from NICU Case Manager
Health Plans
Maternity:
Health plan provides ProgenyHealth with claims/eligibility files
NICU:
Health plan provides ProgenyHealth with notice of admission
Provider
Maternity:
Provider sends referral to ProgenyHealth
NICU:
Facility provides ProgenyHealth with notice of admission

The Employee Advantage
Although many employers now recognize the importance of fertility and family-building benefits, fewer are focusing on the critical need for maternal, postpartum, and NICU care management support.
As employees navigate the highs and lows of pregnancy, postpartum, and parenting, having a trusted partner in the form of a Case Manager, along with the safety net of an end-to-end Maternity and NICU Care Management solution, can make a significant difference in lowering risk and anxiety, while improving employee health outcomes and job satisfaction.
Providing such benefits to a workforce with a clear desire for family-oriented offerings is a recipe for highly competitive talent acquisition and retention. For example, nearly three quarters of surveyed employees say they would switch companies to secure better benefits in this category.
Another study of employed women in the United States showed that women’s healthcare benefits are a major driver in that cohort’s employee retention, with 89% of respondents saying these benefits directly contribute to their job satisfaction and greatly reduce time away from work. Further, that same study revealed the benefits that had the greatest positive effect were those related to mental health, reproductive health, and maternity care.
Solving Quality and Cost with Benefits That Work for Everyone
The message is clear: Employees want to feel safe, cared for, and supported by their benefits package, and family-oriented healthcare benefits play a significant role in achieving this level of satisfaction and security.
Meanwhile, employers are more aware than ever that the twin goals of attracting and retaining talent and maintaining sustainable healthcare costs are essential to thrive in today’s marketplace. Within the space between these two groups is where health plans can provide solutions that don’t just sound attractive, but that truly solve for quality and cost. It’s a rare solution that so resoundingly and simultaneously solves two halves of the same problem—but that’s precisely what a rigorous and integrated maternal and infant care management program accomplishes, delivering on the desires of the workforce and the needs of employers all at once.
ProgenyHealth
ProgenyHealth empowers our health plan and employer partners to change the trajectory of maternal and infant health outcomes across America.
Informed by more than 20 years of experience and patient data, our end-to-end Maternal and Infant Care Management solution helps ensure the best possible outcomes for every expecting mother we touch. Our wholly integrated, tech-enabled solution builds a network of support for an uninterrupted continuum of care from prenatal health, through any resultant NICU stay, and all the way to one full year of life.
From the very beginning, we unite early health risk assessment data with self-directed digital tools and dedicated Case Managers who work tirelessly to connect at-risk moms-to-be with the resources, care, and support they need for a healthier, full-term delivery. Our industry-leading intelligent platform, Baby Trax®, integrates NICU Utilization Management and Case Management, while also driving Payment Validation & Assurance activities based on clinical data. By promoting predictable, equitable, and standardized high quality care journeys, we ensure healthier outcomes—and lower costs—across an entire at-risk population. In so doing, we help overcome systemic barriers to support healthier pregnancies and healthier starts to life for all moms and babies, one family at a time.


